Tag: Metabolic Syndrome
-

Diet Doctor launches Hava.co. Is a satiety score a good thing?
Diet Doctor, long known for it’s advocacy and education surrounding the Keto Diet and living a low carb lifestyle, has launched a new company named Hava. Hava seeks to fill a void for people who feel they can’t sustain a life-long commitment to the Keto Diet by focusing on satiety. This innovative approach and our…
-
Mitochondria dysfunction may be the common denominator between metabolic & mental health problems
Dr. Christopher M. Palmer, a Harvard researcher and psychiatrist, wrote a book called “Brain Energy: A Revolutionary Breakthrough in Understanding Mental Health and Improving Treatment for Anxiety, Depression, OCD, PTSD, and More. Yes, I know, that subtitle is a mouthful. In Brain Energy, Dr. Palmer connects mitochondria dysfunction to mental health issues like Parkinson’s, Alzheimer’s,…
-
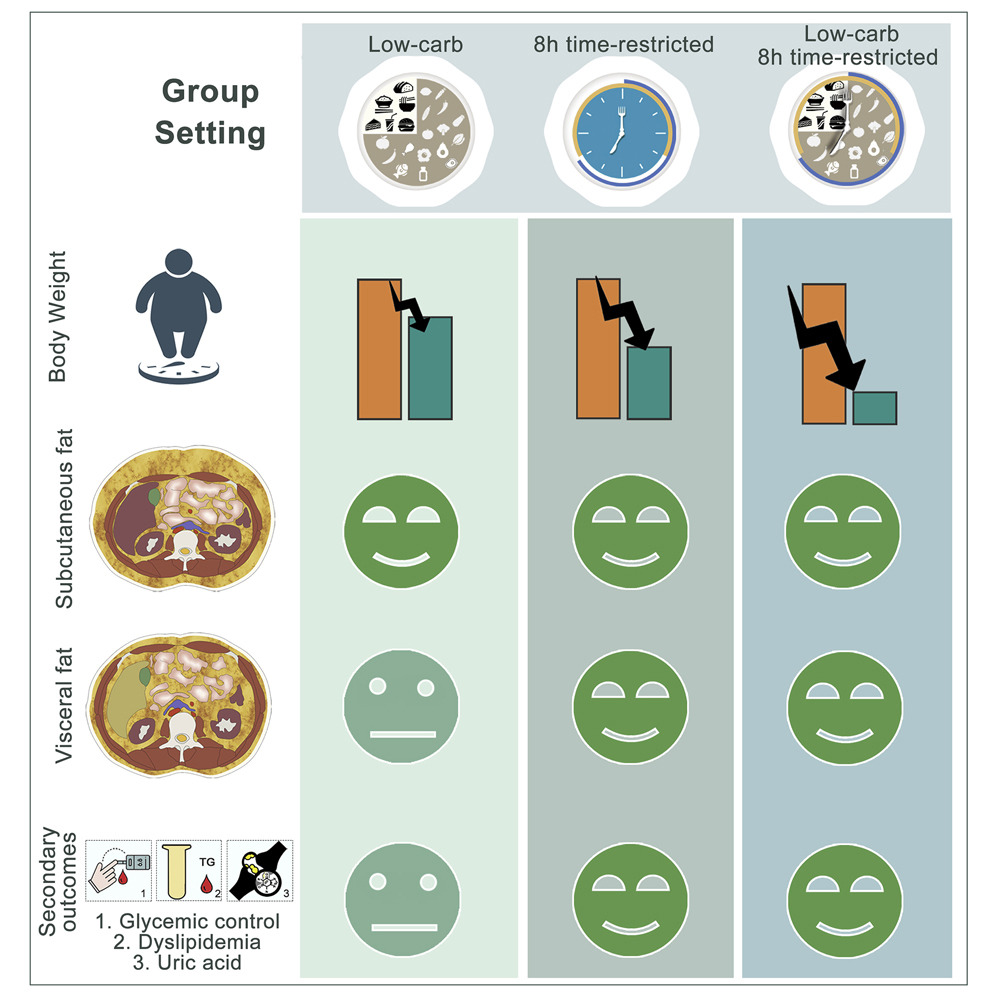
Study: Time restricted eating is an effective intervention for metabolic syndrome
Reducing visceral fat is extremely important. That’s the fat you can’t see. It’s the fat that builds up in your organs and will kill you over time. There is something called “skinny-fat” which describes someone who looks fit or healthy from the outside but has fat surrounding their internal organs. There are so many acronyms…
-

New York Times reports no benefit to time restricted eating… but what did participants in the study eat?
The New York Times reported on a study in the New England Journal of Medicine (NEJM) on time restricted eating, or as it is more commonly known these days, intermittent fasting. It’s important to note the study was also based on calorie restriction, which was left out of the headline, in addition to time restriction.…
-
High Fructose Corn Syrup may block Vitamin D increasing risk COVID-19 infection
It’s increasingly clear that metabolic health and Vitamin D deficiency lead to more serious cases of COVID-19. Obviously I’m not a doctor but when I heard the information in this post I had to pass it along. I ran across the following recording of Dr. Roger Seheult of MedCram.com. In this audio he explains how…
-
Study: Metabolic Syndrome on the Rise
Some of the unchanging facts during the COVID-19 pandemic is that most of the people that are having severe reactions and having difficulty recovering are those with metabolic syndrome. What is metabolic syndrome? Metabolic syndrome is a clustering of at least three of the five following medical conditions: abdominal obesity, high blood pressure, high blood…
